Read the first part of Tanya’s Pregnancy Journey Living with Crohn’s Disease in India on SAIA’s blog: https://southasianibd.org/tanyas-pregnancy-journey-living-with-crohns-disease-in-india/
I put off writing this blog for the longest time… I did not know how to write it.
In many ways, I didn’t actually want to write it. I felt ashamed to be feeling the things I felt. I kept deleting draft after draft because it felt self-indulgent to ‘feel’ those things and the last thing I wanted was to admit these feelings to the world. In a culture where we are taught to always count our blessings and experience gratitude and thankfulness every day, sometimes…. we mask our true selves and our real feelings so much that even ‘we’ are unable to see it.
A veil of ‘pseudo-optimism.’
Pregnancy is a very special journey. For nine months, both of you tenderly, carefully nurture the unborn child in your womb. You admire his little movements at every scan, you are curious about this little life form you have created at every visit to the gynaecologist. You are diligent, sincere, hopeful parents researching and asking questions even before you become parents. At the end of the journey, you have a beautiful baby in your arms: a new connection, a new bond, an entire new generation created from your cells.
A mother is born.

I vividly remember the day I brought my baby home for the first time. It was twelve whole days after he was born. The journey from womb to home had been nothing short of traumatic. I had delivered a healthy baby boy on a beautiful Sunday morning, a full-term, smooth, uneventful pregnancy leading to a planned C-section surgery. Everything seemed to be going so smoothly. What happened shortly after his birth though, could not have been more different and disturbing. The breathing complications of pulmonary hypertension that my baby developed, resulting in hospitalization, intensive care treatment and ventilator use and the ‘ill-informed’ advice to de-escalate my Crohn’s medication have already been dealt with in my previous blog post: https://southasianibd.org/tanyas-pregnancy-journey-living-with-crohns-disease-in-india/
I am standing on the doorstep of the house I grew up in as a teenager. But I am not alone; I am holding my twelve-day old baby, tightly swaddled in a soft cotton saree. My mother, a newly minted grandmother, nervously swirls the traditional drishti plate with vetrilai, chunambu and lit camphor around me and the baby, warding off any evil from entering the house with us. I walk into my parents’ home filled with a sense of relief, tinged with happiness, hope and the incomparable feeling of the weight of this tiny little baby in my arms.
The past 12 days seemed unreal, like a bad dream of hospital visits and monitors beeping and a tiny little infant connected to tubes. I allowed myself to finally breathe, but my mind kept going back. As the ‘mother’ I was the only one permitted to hold my baby in the NICU; albeit fleetingly, to encourage skin to skin contact. I would need to sign a register before entering the NICU, and I always wondered about the other signees in that book, names that didn’t register because of my tears. Our families had rallied around us night and day at the hospital, throughout this nightmare- bringing us tea and idly, offering to drive us home, offering to stay through the night so we could get some sleep. Given the trauma of his birth and the emotional turmoil that followed, we were all understandably exhausted and spent, both physically and emotionally.
Now that the healthy duo of mother and child were safely back home, in-laws, parents and my husband each went their respective ways to get much needed rest and sleep. I was left alone with my baby. The natural conclusion would be that mother and baby connected instantly, and the joy of motherhood would have healed all my wounds and scars. But the usual teething time new mothers get with their babies in the hospital was a luxury completely cut out for me. The moment he was born, he was shifted to the NICU where he fought valiantly for eleven days. As soon as he was strong enough to be moved off the ventilator, he was cleared for discharge so he could be rushed off to an infection free environment at home. There was no experienced nurse to teach me how to gently cradle his neck while teaching him to suckle. Now all alone with him for the first time, I was scared, lonely and unsure of myself.
I was anxious if he was getting enough milk. I was anxious if I was producing enough milk. I was anxious if he was peeing enough and if he was pooping enough. I was anxious if my milk had enough nutrition. I was anxious that I would sleep and not hear him cry. I was anxious to catch up on sleep whenever he slept. Was he sleeping enough? Was he gaining enough weight? Was I feeding from both breasts alternately, as I was advised to? I so desperately wanted to rest, but I was too wired to fall asleep. I would wake up with a start to imaginary crying and would find it hard to go back to sleep. It seemed relentless, day and night, night and day on call. I was fatigued to my bones. When he cried, I would try nursing him, rocking him, burping him, cuddling him, and walking with him. Nobody else seemed to find him exhausting. Nobody else complained. Nobody else seemed to tire of him. Nobody else hated the sound of his crying.
The level of interaction with my GI and gynaecologist when I was pregnant, dropped drastically after I delivered. They wanted to give me breathing space with the demands of the new baby. When you are pregnant and carrying a life form within you, there is considerable focus on your physical and emotional wellness – Lamaze breathing techniques, maternity yoga, birthing position classes, even lactation simulation classes, the list of pre-skills seemed to be endless. Nothing prepares you though, for the postpartum exhaustion of being overwhelmed daily.
If my friends had to find three words that defined me, ‘nurturing’ would be top on that list. So, it baffled me that I was unable to nurture the one being that needed me the most. I tried to be cheerful. I tried to recalibrate what I had been gifted with. I had a beautiful little baby boy whose life I was most grateful for. Yet, I found it hard to connect to this person who seemed to drain me from within. I couldn’t connect with my family or my friends who were also new mothers. The hormonal changes in my body left me emotionally disconnected and depleted. I was sleepy, irritable and miserable 24/7.
We idolize motherhood. We symbolize it as the epitome of selflessness. I was unable to detach my needs from my responsibilities and duty. I was ashamed to admit, even to myself, that the primal urge to nurse and care for one’s baby did not seem to bring me joy. I was unable to prioritize my body and my health. The exhaustion, the lack of sleep, the continuous anxiety and the stopping of my Crohn’s medication all quickly piled up, and I was hurtling rapidly toward a flare. My ‘go-to caregivers,’ my husband and my mother, were busy fussing over the demands of the new baby. I was not conditioned to ask for help or cry for attention. I was the mother, not the baby!
If you are reading this blog, you know from personal experience that handling a Crohn’s flare up is never straightforward. Prioritizing sleep, getting enough rest, and minimizing stress are often the top three suggestions on health blogs to help manage Crohn’s flares. Apart from this, there was a clear need to reassess my course of treatment. The whole exciting cycle of monitoring symptoms, evaluating blood parameters, trying out a different level of medication, watching for symptomatic improvement, amping up the dosage, tapering off the steroids and hoping for the symptoms to subside with every advanced treatment therapy — we’ve all been down that road, some of us more often than we’d like. Recovering from a flare is massively stressful by itself. But unlike other times before my postpartum flare, I couldn’t JUST be a patient recovering from an IBD flare up. I couldn’t put my feet up and prioritize rest, sleep and medication. There was a living crying human who was dependent on me. I had no time for selfcare or rest. I felt like I was falling into an abyss without a harness. While the actual process of getting pregnant and having a baby took less than a year, recovering from my postpartum flare took me nearly 2 years.
In this period, I felt I had lost control of everything, my health, my sleep, my routine and even my appearance. I shed my pregnancy fat in a few weeks, but the breast-feeding weight took a little longer. However, the most stubborn was the unseemly steroid-induced fat. There were times when I refused to be photographed with my baby because I was repulsed by how I looked.
What should have been a happy time of bonding was both demanding and stressful emotionally. In hindsight, of course, I wish I had recorded every moment of that journey. But my mind was unclear, I was not thinking straight. I was going through a form of postpartum depression and was simply unaware of it. I was exhausted every day but felt too guilty to complain. I was crying internally for help, but too ashamed to say I could not manage. I was lonely, even while holding my baby.
Studies show that women with IBD have an increased risk of postpartum disease activity, especially those who have had a history of disease complications or when advanced therapies including biologics are de-escalated during or after pregnancy. Studies have also showed that women with IBD have an increased risk of developing postpartum depression and anxiety and this increased risk is multifactorial – in part due to biological changes and in part due to psychosocial changes of adjusting to the demands and challenges of motherhood. Cognisance of this risk, among both patients and providers as well as early identification and treatment could make this period smoother for the families involved and a lot less lonely for the mother and improve her healthcare outcomes and support the baby’s development.
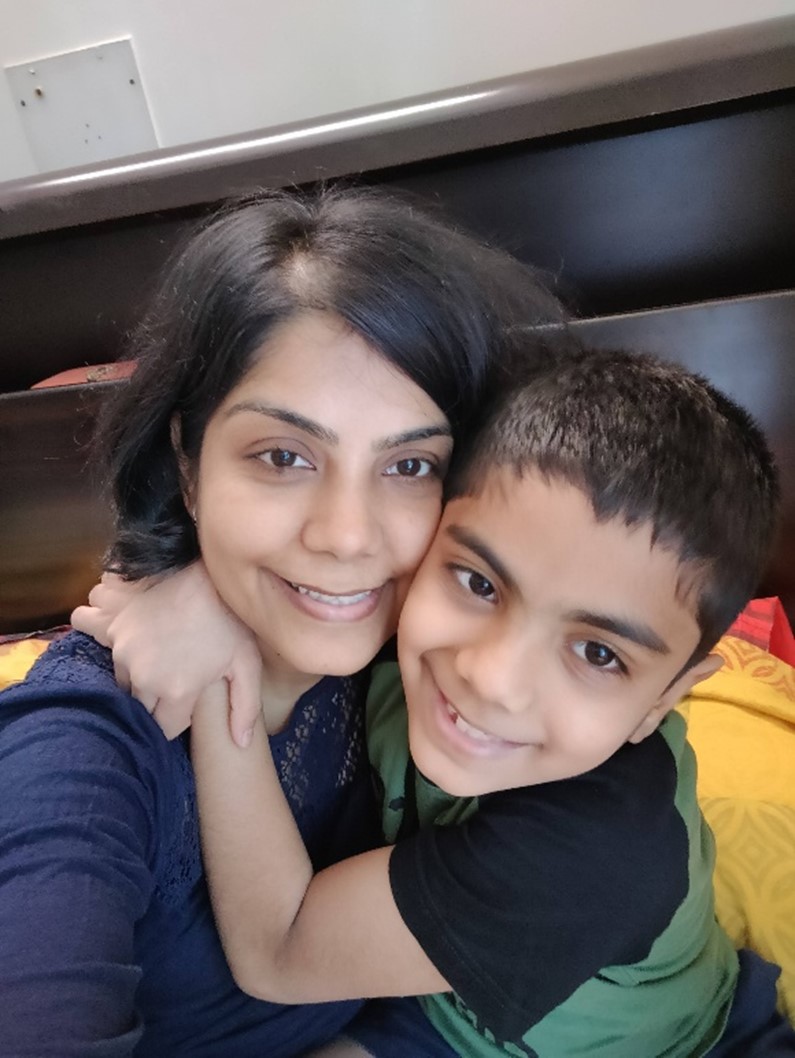
In my case, the bond grew gradually and beautifully. The connection I longed for with my child came with time, as I got more rest, found the right treatment for my IBD, and as he began sleeping better and responding more to the world around him.


As things settled, I found myself more present and able to give him the love and attention I had always wanted to. We built cars and garages out of cardboard, imagined jungles and tigers, devoured books and facts, matched each letter of the alphabet with a dinosaur, and studied the tiniest insects. We invented board games, shared endless laughs, and made memories that brought us closer together.
He is almost ten now, and nothing brings me more joy than watching him grow, hearing his stories from school, engaging with his beautiful mind, and feeling my heartbeat outside of me daily.
In spite of IBD and the post-partum mental health challenges I experienced, my family and I were able to build a beautiful life together. I wish the same for our community and encourage others to seek help and for our doctors to ask us how we are doing beyond our pregnancy, labor and delivery journey.

RESOURCES ON PREGNANCY & FERTILITY IN IBD & OSTOMY/JPOUCH SURGERY
To watch Facebook Live discussions by South Asian IBD Alliance, on Pregnancy & Fertility in IBD & Ostomy/J-Pouch Surgery, visit our YouTube channel: https://youtu.be/ppvTutTH-IQ
To contribute to the PIANO study and advance understanding of advanced therapies in IBD during pregnancy, please visit https://pianostudy.org/
Other resources for pregnancy after IBD surgery (ostomy & j-pouch) from United Ostomy Associations of America: https://www.ostomy.org/pregnancy/, https://www.ostomy.org/labor-delivery-with-ostomy/ & from Crohn’s and Colitis Canada: https://crohnsandcolitis.ca/About-Crohn-s-Colitis/IBD-Journey/Fertility-and-Pregnancy-in-IBD/Factors-That-Can-Affect-Fertility#:~:text=Women%20with%20IBD%20have%20the,or%20previously%20having%20pelvic%20surgery.
IBD pregnancy & fertility nonprofits & advocates to follow include: AGA’s The Parenthood Project, IBD Moms, Natalie Hayden of Lights, Camera, Crohn’s & Jessica Caron of Chronically Jess.
