
Written By Madhura, Basmah, Nour & Demi
Reviewed by Tina Aswani-Omprakash
Our patient advocate team, SAIA’s IBDesis, was honored to attend Digestive Disease Week (DDW) between May 4 – 6th, 2025, in San Diego, California. DDW 2025 allowed us to learn more about the latest research and developments in the GI space. We are excited to share our learnings and key takeaways from the conference with our patient community!
AGA’s Living Guideline for Crohn’s Disease (Madhura Balasubramaniam)
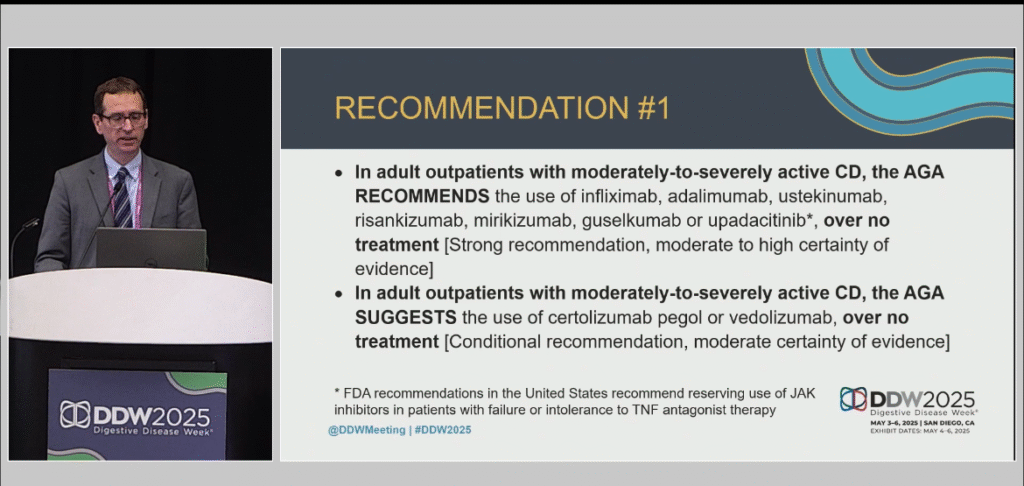
At DDW 2025, leading researchers presented the American Gastroenterological Association’s (AGA) Living Guideline for Moderate-to-Severe Crohn’s Disease. Based on robust data, the guideline grouped the available medications into different baskets based on their effectiveness. This will help physicians decide how to prescribe specific medications for patients like us with moderate to severe Crohn’s disease. Since this is a living guideline, the clinician committee working on the guideline will review new research every 6 months and update the guideline regularly. The committee also intends to seek input on the guideline from other doctors and patients.
Why does the guideline matter for us patients?
- Many new treatment options have been approved for managing Crohn’s Disease in the last few years, including IL23 drugs such as guselkumab, mirikizumab, and risankizumab and JAK inhibitors like upadacitinib. The guideline addresses these new treatment options and provides recommendations on how to position these medications and when to use specific medications over others. This provides us with evidence-based inputs on the treatments and combination of treatments that can help us get our Crohn’s under better control.
- We now have many highly effective treatments for patients who have never been on a biologic before (bio-naïve patients) as well as those who have been on advanced therapies before. Knowing this information allows doctors to choose the appropriate therapy for each of us, depending on our treatment history. This is important for us patients because even those of us, for whom previous treatments have not worked well, now have more options to manage our disease effectively.
- The guideline recommends that patients be on any effective medication rather than no treatment. As patients, we must remember that not treating moderate-to-severe Crohn’s Disease may come with risks and may lead to complications and adverse outcomes.
- We must work with our doctors and decide which medications to use through shared decision-making. This is an empowering process where we as patients and our treating doctors come together to make treatment choices. Here, along with scientific and clinical evidence, our preferences and considerations as patients play an important role in deciding the right treatment for us at a given point in time.
In addition to many sessions on IBD medications and their various mechanisms of action (how the medications work), DDW 2025 had a strong whole-person perspective and had sessions on the role of diet in GI conditions.
The Role of Diet in Managing GI Conditions (Basmah Ali)
At Digestive Disease Week in San Diego, I had the privilege of attending a session about one of the most enthusiastically discussed topics amongst patients – diet. Doctors addressed low FODMAP, gluten-free, low-carb, and Mediterranean diets that impact people with irritable bowel syndrome (IBS). Since many of us with Crohn’s disease or ulcerative colitis also experience IBS, we should pay attention to the research! Here are some of the takeaways:
- All the different diets provide some degree of symptomatic relief for IBS patients.
- With diets that eliminate whole food groups, there are risks such as malnutrition, potential eating disorders, and food insecurity.
- While some percentage (16-30%) of patients in clinical trials for non-celiac gluten sensitivity had a true reaction to gluten, others more likely had symptoms due to FODMAP content in the food.
- The Mediterranean diet may be considered an alternative to other diets that focus on restriction as it gives many of us various options of food that we can eat rather than foods we must restrict.
- Regardless of the dietary approach, it is imperative to include an expert dietitian focused on gastroenterological conditions and an adequate support system to optimize quality of life for patients.
Growing up in a culture that centers events around people and food, managing dietary restrictions and cultural expectations is challenging to navigate. We need more research on tailoring specific cuisines to provide culturally sensitive care for IBS and IBD patients. I am excited for the day that we can enjoy food while maintaining our health, sense of community, and sense of self!
When Food Mirrors Migration (Demi Ricario)
At Digestive Disease Week 2025, I attended a session that felt like it was written with my story in mind: Diet and Nutritional Selection of the Gut Microbiome Composition in Gut Health and Disease. Dr. Siew Chien Ng, from the Chinese University of Hong Kong, presented compelling insights on how migration from non-Western to Western diets may disrupt the gut microbiome and trigger inflammatory bowel disease (IBD).
She outlined four epidemiologic stages of IBD and explained how globalization and urbanization are accelerating the global rise of IBD. Diets high in fat, sugar, and food additives, which are increasingly common in Westernized diets, can profoundly alter our gut microbiota.
Why does this matter to us as patients? As people migrate, their diets often shift. More processed options replace traditional, whole-food meals. This dietary change mirrors the migration journey, moving from East to West or rural to urban life. Just like migration brings both opportunities and challenges, this shift in diet may have profound effects on our gut health.
This presentation hit home for me. I moved from the Philippines to the U.S., and within eight years, I was diagnosed with ulcerative colitis. Even today, removing heavily processed Western food during a flare and returning to simpler, more traditional meals often helps calm my symptoms.
What struck me most was her explanation that some gut bacteria are both heritable and sensitive to diet.
In other words, we may inherit certain gut bacteria from our parents, much like our eye color or bone structure. But that’s not the end of the story. These same bacteria are highly responsive to what we eat, especially during critical timeframes or “windows” when our microbiome is more open to change, such as during migration, illness, or life transitions.
This creates a therapeutic opportunity: if we understand how to target both the “seed” (our genes) and the “soil” (our diet and environment), we could prevent or even manage diseases like IBD more effectively.

Dr. Ng’s research didn’t just validate my lived experience. It pointed toward a hopeful roadmap. Understanding that our gut health is shaped by both heritage and habits empowers us to make choices that support remission, resilience, and a better quality of life.
Several sessions and posters at DDW 2025 focused on social determinants of healthcare and the importance of improving access to GI care for all patients.
Reducing Disparities and Improving GI Care for All (Nour A)
Dr. Rachel Issaka provided insightful information about obstacles and challenges Native American communities faced in accessing IBD care.
A key focus was on colorectal cancer screening. The research found that only 56% of patients with abnormal stool tests complete follow-up colonoscopies within a year. This number often dropped as low as 18% in some safety-net systems. This is very concerning because research shows that there was a two-fold increase in mortality among individuals who have abnormal stool tests but did not complete a follow-up colonoscopy.
What is worse is that despite the high disease burden in their communities, American Indian and Alaska Native populations remain severely underrepresented in these studies—less than 0.5%.
Dr. Issaka pointed to several barriers to care for these communities, including health system fragmentation, delays in communicating abnormal results, fear of procedures or diagnosis, and lack of transportation.
The presentation identified several solutions to these challenges, including:
- Patient Navigation Programs (improved follow-up colonoscopy rates by 14% on average)
- Partnerships with rideshare platforms like Uber or Lyft to reduce transport barriers and provide safe and cost-effective rides for patients who may not be able to access it otherwise.
- Video Aids reduce fear around procedures and help patients understand the importance of colonoscopies.
The key take-home message for me from this session was that there’s no one-size-fits-all approach to address these barriers. We need tailored, community-driven interventions and culturally responsive strategies to address the specific needs and concerns of the community, close these gaps, and ensure high-quality and accessible GI care for all patients.
Poster Session: Biologic Therapy Initiation is Delayed in Pediatric South Asian IBD Patients in the United States (Madhura Balasubramaniam)
Like Dr. Issaka’s presentation, the poster by Tandon, Bachand, and Yegembayeva et al. found a significant delay in starting biologics in pediatric IBD patients of South Asian origin in the US. The poster reported that despite having more severe upper GI disease, elevated biomarkers, and weight loss, South Asian pediatric IBD patients do not start a biologic on time. Instead, South Asian pediatric patients explore complementary and alternative therapies like Ayurveda or Homeopathy first or forgo treatment altogether.
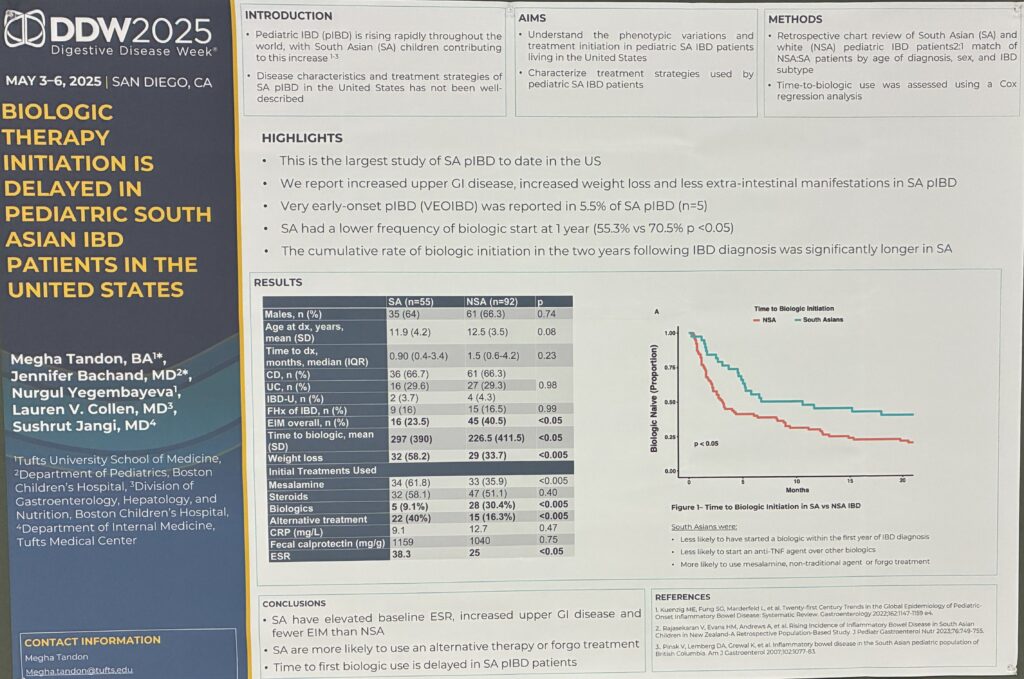
This poster points to the cultural barriers that many patients from different communities experience and how these can lead to alarming delays in care and poorer disease outcomes. Through our patient education efforts and patient support group, IBDesis Community, SAIA plays an essential role in breaking this stigma around effective medications and supporting patients as they navigate these cultural norms and barriers.
Concluding Thoughts
As patient advocates, we were grateful to attend DDW and learn from the leaders in the IBD and GI space. From SAIA & AGA’s Clinical Research Roundtable, the Bridging the Communication Gaps event hosted by Monday Night IBD, SAIA, and COGI to the multiple conference sessions, DDW 2025 was a phenomenal learning experience for all of us. It reminded us of how far we have come and how much further we still must tread to elevate care for all individuals living with GI conditions.
